Understanding Laser Eye Treatment: Types, Benefits, Risks, and Recovery
Outline
– How laser vision correction reshapes the cornea to focus light accurately
– Key procedure types and how they compare: PRK, LASIK, and SMILE
– Eligibility, screening tests, and who should wait
– Expected results, risks, and long-term considerations
– Preparation steps, recovery timelines, and aftercare tips
Introduction
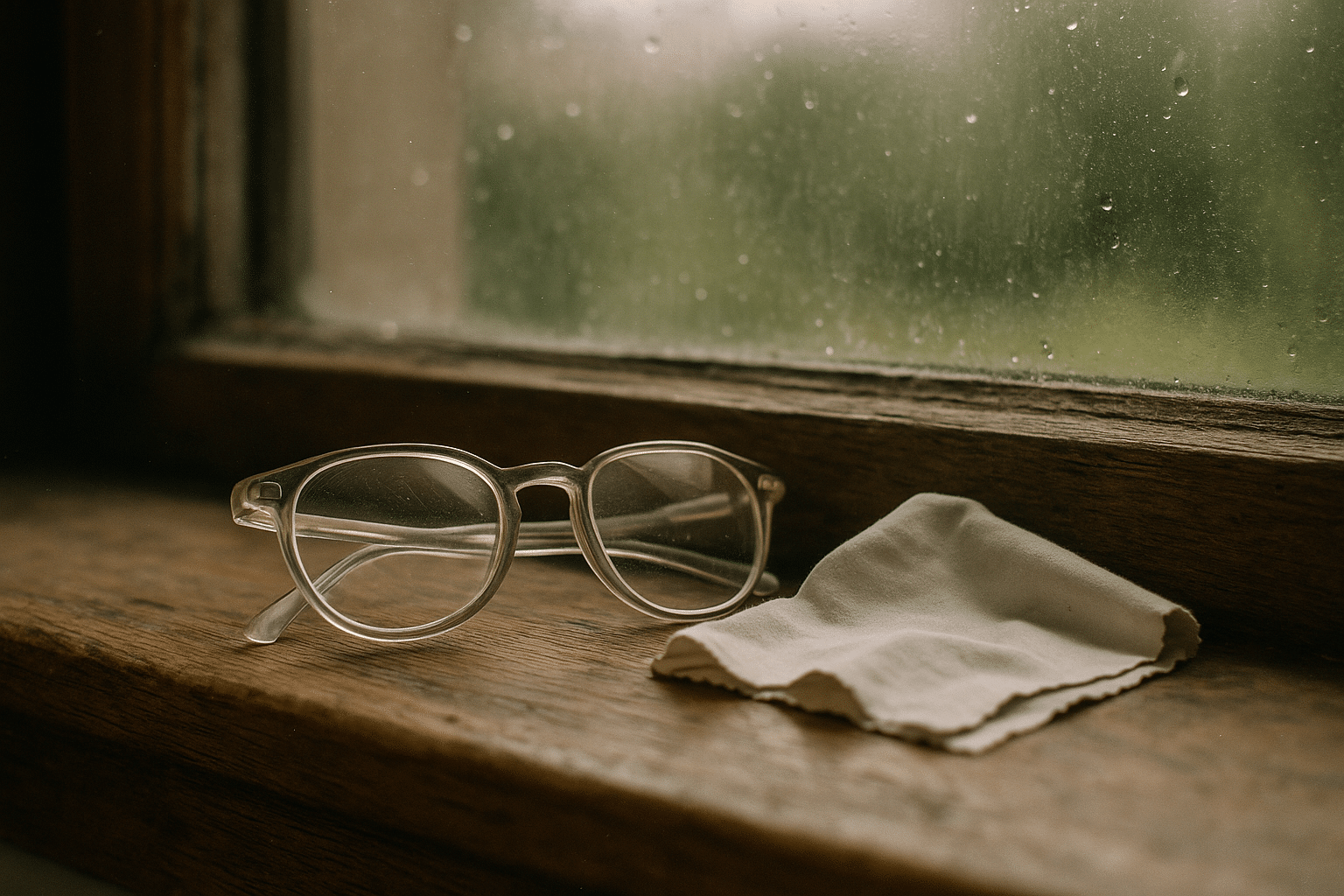
For many people, glasses and contact lenses are reliable companions, but they can also be inconvenient, costly to maintain, and limiting during sports or travel. Laser eye treatment offers an alternative by reshaping the cornea so light focuses crisply on the retina. It has matured over three decades, supported by extensive clinical data and evolving technology that emphasizes precision and safety. Still, it is not a one-size-fits-all solution. This guide explains how the procedures work, who qualifies, what outcomes to expect, and how to approach recovery with patience and care, so you can make a grounded decision that fits your eyes and your lifestyle.
How Laser Vision Correction Works: From Light to Focus
Laser eye treatment improves focus by subtly reshaping the cornea, the clear, dome-shaped front surface of the eye. In simple terms, the cornea acts like a camera lens; if its curvature doesn’t match your visual needs, images land in front of or behind the retina, creating blur. The treatments most people consider target common refractive errors: myopia, hyperopia, and astigmatism. Using laser energy, microscopic layers of corneal tissue are removed or redistributed to change curvature by just the right amount. The typical cornea is about 500 to 560 microns thick; for context, a single human hair sits in a similar range. Laser reshaping is measured in microns, often around 12 to 16 microns of tissue per diopter of correction, though exact figures vary with algorithms and optical zones.
Two key laser types are used. The excimer laser emits ultraviolet light to precisely ablate tissue without heating, a process that “cold-sculpts” the cornea. The femtosecond laser creates ultrafast pulses that separate tissue by forming microcavitation bubbles, allowing surgeons to create a corneal flap or a lenticule, depending on the chosen procedure. Modern systems pair these lasers with active eye-tracking to maintain alignment even if micro-movements occur during the seconds-long treatment. Many platforms also use wavefront or topography-guided planning, which maps subtle optical imperfections—known as higher-order aberrations—to tailor the reshaping in a more personalized way.
While the engineering is intricate, goals remain practical: improve uncorrected distance vision and reduce dependence on external lenses. Results rely on careful selection and sound measurements, including accurate refraction, corneal thickness, curvature patterns, and tear film quality. Consider these core components that shape outcomes:
– Corneal thickness and shape: They set the safe margin for tissue removal.
– Optical zone size: Larger zones can help with night vision but require more tissue.
– Tear film stability: Dryness can blur measurements and recovery.
– Precision tracking and planning: Reduce alignment and optical quality issues.
When all elements align, laser correction can deliver crisp daytime vision and reliable night performance. Yet the same precision that makes it compelling also demands thorough screening and realistic expectations, topics explored in the next sections.
Comparing Procedures: PRK, LASIK, and SMILE at a Glance
Although laser eye treatment is often used as a blanket term, the techniques differ in how they access and reshape the cornea. PRK, LASIK, and SMILE share the same goal—clearer focus—but they get there via distinct paths, each with trade-offs in comfort, recovery speed, and biomechanical considerations.
PRK, or surface ablation, removes the thin epithelial layer on top of the cornea before the excimer laser sculpts the stromal bed. The epithelium then regenerates over several days. This approach preserves more corneal tissue depth because it creates no flap, a point valued for patients with thinner corneas or certain shape profiles. However, early recovery often includes light sensitivity and discomfort for a few days, along with a slower return to crisp vision—commonly one to three weeks for stable clarity. PRK can be a thoughtful choice when corneal thickness or lifestyle factors (like risk of eye trauma) make flapless options appealing.
LASIK involves creating a thin corneal flap using a femtosecond laser, lifting it to allow excimer treatment on the underlying stroma, and then repositioning the flap. Many patients appreciate the rapid visual recovery—often functional within 24 hours and refining over a week—and minimal early discomfort. The trade-off is the presence of a flap, which slightly alters corneal biomechanics and introduces a small risk of flap-related issues. For everyday life, this is usually a minor consideration, but those in contact sports or occupations with risk of direct eye impact may favor flapless approaches.
SMILE uses a femtosecond laser to create a lenticule within the cornea and a small incision to remove it, changing curvature without a large flap or surface removal. Early comfort can be favorable, and some evidence suggests a lower incidence of early dry eye symptoms compared with flap-based methods, likely due to reduced disruption of corneal nerves. Visual recovery is generally quick, though fine-tuning astigmatism may be less flexible than with excimer-sculpted profiles, depending on individual anatomy and technology generation.
In practice, the “right” method depends on your eyes and priorities:
– PRK: No flap, tissue-sparing, slower comfort and clarity early on.
– LASIK: Swift clarity, comfortable early recovery, includes a flap.
– SMILE: Small incision, potentially less early dryness, nuanced astigmatism handling.
All three can yield excellent vision in suitable candidates. The decision hinges on corneal maps, thickness, prescription range, tear stability, and lifestyle—elements your evaluation will bring into focus.
Who Is a Good Candidate—and Who Should Wait
Eligibility for laser eye treatment balances the desire for clearer vision with the anatomy and health of the eye. Ideal candidates are adults with a stable prescription, healthy corneas, and realistic expectations about outcomes and side effects. Generally, stability means minimal prescription change—often defined as less than 0.50 diopters—over 12 months. Age matters because early adulthood can still bring shifts in refraction; many clinics suggest waiting until at least your early to mid-20s unless special circumstances apply. Accurate preoperative measurements underpin success, so contact lenses may need to be paused for days to weeks before testing to avoid warping corneal shape.
Several factors can steer a person toward or away from specific procedures. Thinner corneas or irregular patterns on topography may favor surface-based options. Marked dry eye symptoms at baseline can complicate both measurement and recovery, so treating the tear film first can improve accuracy and comfort. Pregnancy and breastfeeding often prompt deferral due to hormonal shifts that alter corneal hydration and prescription stability. Autoimmune conditions, uncontrolled diabetes, active eye inflammation, or a history of corneal ectatic disorders such as keratoconus can increase risk; specialized evaluations and alternatives may be more suitable in those cases.
During screening, expect a comprehensive workup. Core elements often include:
– Refraction checks to confirm stability and accuracy.
– Corneal topography and tomography to assess shape and rule out ectasia risk.
– Pachymetry to measure thickness and preserve a safe residual stromal bed.
– Pupil size evaluation to help optimize night vision planning.
– Tear film and meibomian gland assessment to address dryness beforehand.
Some patients benefit from discussing nuanced strategies such as monovision, which sets one eye for distance and the other for near to offset presbyopia. This can be tested with contact lenses before any permanent change. Others may learn that a non-laser solution—like phakic lens implantation or refractive lens exchange—better fits their prescription or corneal profile. The key is a candid conversation about goals, daily visual demands, and tolerance for trade-offs. If any red flags appear during testing, waiting and treating underlying issues can transform an uncertain plan into a confident one.
Expected Results, Risks, and Long-Term Considerations
Outcomes for modern laser eye procedures are generally strong in appropriately selected candidates. Many studies report that a high proportion of patients—often around 90 to 95 percent in certain groups—achieve 20/20 or better uncorrected distance vision after LASIK, with PRK and SMILE showing comparable performance in similar ranges when matched for prescription and corneal health. It’s important to remember that statistics summarize groups; individual results vary based on prescription magnitude, corneal shape, healing patterns, and dry eye tendencies. Enhancements, or touch-ups, are sometimes needed—figures commonly range from about 1 to 5 percent depending on age, baseline prescription, and time since surgery.
Side effects are part of the informed consent conversation. Temporary dry eye symptoms are common in early recovery, usually improving over weeks to months as nerves regenerate and the tear film stabilizes. Some patients notice halos or glare in low light, especially in the first few weeks; careful planning of optical zone size and management of dryness can mitigate this. Flap-related issues in LASIK are uncommon, and corneal ectasia—progressive thinning and bulging—remains rare with modern screening but is a serious consideration, underscoring why topography and tomography matter.
Long-term, most patients enjoy stable distance vision, but eyes continue to age. Presbyopia, the gradual loss of near focus typically starting in the 40s, will still emerge because it arises from the lens inside the eye rather than the cornea. Options to address near tasks later include readers, monovision strategies, or future lens-based procedures. Another practical factor is cost. Prices vary by region, technology, and clinic, and can include preoperative testing, postoperative visits, and enhancement policies. While upfront costs can be significant, many people compare them with years of lenses, solutions, and frames to evaluate value.
Keep expectations grounded with a simple checklist:
– Aim for reduced dependence on glasses rather than a guarantee of perfect vision.
– Expect temporary dryness and night symptoms that usually fade with time.
– Plan for follow-up visits and potential enhancements if minor residual error persists.
– Remember presbyopia will still arrive with age, regardless of laser correction.
With clear goals and a careful workup, laser eye treatment can offer dependable clarity for daily life, while a measured understanding of risks helps you navigate the journey confidently.
Preparation, Procedure Day, and Recovery Timeline
Preparation sets the tone for accurate measurements and a smoother recovery. If you wear soft contact lenses, you may be asked to stop for about a week before final measurements; rigid or scleral lenses often require longer breaks to let the cornea return to its natural shape. Managing dryness beforehand—using preservative-free lubricants, warm compresses, and eyelid hygiene—can improve both testing precision and early comfort. Plan transportation on procedure day, avoid eye makeup, and keep caffeine modest to minimize sensitivity. A calm, well-rested approach helps more than you might expect.
The procedure itself is typically brief. You’ll lie under the laser while the team confirms alignment, and you may hear clicking or notice a mild pressure sensation for a few seconds. Treatment time per eye is often under a minute, with total room time around 10 to 20 minutes for both eyes. Afterward, expect protective shields and a clear drop schedule that might include antibiotics, anti-inflammatories, and lubricants. Sunglasses help with light sensitivity on the ride home, and most people appreciate a nap as the numbing drops wear off.
Recovery timelines differ by method:
– PRK: Expect 3 to 5 days of notable light sensitivity and grittiness while the surface heals, with clarity improving over one to three weeks and refining over one to three months.
– LASIK: Many people see functional vision within 24 hours, with finer detail sharpening over days; mild dryness is common early on.
– SMILE: Vision usually clears quickly, with early comfort often favorable; refinements continue for several days to weeks.
General rules of thumb support healing. Avoid eye rubbing, heavy sweat dripping into the eyes for a week, swimming or hot tubs for about two weeks, and eye makeup for roughly a week. Keep water out of the eyes in the shower during the first few days. Use lubricating drops as advised, especially during screen-heavy days. Red flags that warrant a prompt call include sudden pain, a marked drop in vision after initial improvement, increasing redness, sensitivity to light, or discharge. A typical follow-up schedule includes day one, week one, and one to three months, but your plan may vary with individual needs.
Finally, give your eyes grace. Vision can fluctuate as the cornea and tear film stabilize, and night halos tend to fade as healing progresses and the brain adapts. Quality rest, hydration, and adherence to the drop regimen create a steady runway to stable clarity.
Conclusion: A Clearer Path, Chosen Carefully
Laser eye treatment can simplify daily life, but the winning strategy is thoughtful selection rather than speed. If you value clear distance vision without constant reliance on lenses, take time to confirm candidacy, compare procedures, and map your recovery. Ask about corneal thickness, optical zone planning, dryness strategies, and enhancement policies, and weigh them against your lifestyle and work demands. With a measured approach—and a clinician who explains every step—you can choose a path that fits your eyes, your goals, and your peace of mind.